
Risk tolerance in healthcare sets the stage for this enthralling narrative, offering readers a glimpse into a story that is rich in detail with casual formal language style and brimming with originality from the outset.
As we delve into the realm of risk tolerance in healthcare, we uncover the intricate balance between managing uncertainties and ensuring quality patient care.
Risk Assessment in Healthcare
Conducting risk assessments in healthcare settings is crucial to ensure the safety of patients, healthcare professionals, and the overall quality of care provided. By identifying potential risks and taking proactive measures to mitigate them, healthcare organizations can prevent adverse events, improve patient outcomes, and maintain a safe environment for all stakeholders.
Common Risks in Healthcare
Healthcare professionals need to assess a variety of risks in their daily practice, including but not limited to:
- Patient falls
- Medication errors
- Healthcare-associated infections
- Surgical complications
- Documentation errors
Identifying, Analyzing, and Evaluating Risks
The process of risk assessment in healthcare involves:
- Identifying Risks: This step requires healthcare professionals to recognize potential hazards or vulnerabilities that could lead to harm.
- Analyzing Risks: Once identified, risks need to be thoroughly analyzed to understand their impact, likelihood, and root causes.
- Evaluating Risks: After analysis, risks are assessed based on their severity and likelihood of occurrence to prioritize them for mitigation strategies.
Risk Management Strategies
Risk management strategies in healthcare play a crucial role in ensuring the safety of patients, staff, and the organization as a whole. These strategies help identify, assess, and mitigate risks that may impact the quality of care provided. Let’s delve into the different risk management strategies employed in healthcare.
Proactive Risk Management Approach
Proactive risk management involves identifying potential risks before they occur and taking steps to prevent them. This approach focuses on implementing policies, procedures, and training to minimize the likelihood of adverse events. By promoting a culture of safety and continuous improvement, proactive risk management aims to address issues before they escalate.
- Regular risk assessments to identify potential hazards and vulnerabilities.
- Implementing quality improvement initiatives to enhance patient safety.
- Providing staff training on best practices and protocols to prevent errors.
- Utilizing technology for early detection of risks and monitoring of patient outcomes.
Preventive measures are key in proactive risk management to reduce the chances of adverse events.
Reactive Risk Management Approach
Reactive risk management, on the other hand, involves responding to risks after they have occurred. This approach focuses on incident reporting, root cause analysis, and corrective actions to prevent similar events in the future. While reactive risk management is essential for addressing immediate concerns, it is often seen as less effective than a proactive approach.
- Incident reporting systems to capture and analyze adverse events.
- Root cause analysis to identify the underlying factors contributing to incidents.
- Implementing corrective actions and process improvements based on findings.
- Sharing lessons learned to prevent recurrence of similar incidents.
While reactive risk management is necessary, combining it with proactive strategies can enhance overall risk mitigation efforts.
Role of Technology in Risk Management
Technology plays a significant role in enhancing risk management practices in healthcare. From electronic health records to advanced analytics tools, technology enables organizations to identify, track, and address risks in real-time. By leveraging data-driven insights and predictive analytics, healthcare providers can proactively manage risks and improve patient outcomes.
- Electronic health records (EHRs) for comprehensive patient information access.
- Real-time monitoring systems to track patient status and vital signs.
- Predictive analytics tools to forecast potential risks and prevent adverse events.
- Telemedicine platforms for remote consultations and monitoring of patients.
Integration of technology in risk management not only enhances patient safety but also improves operational efficiency and decision-making processes.
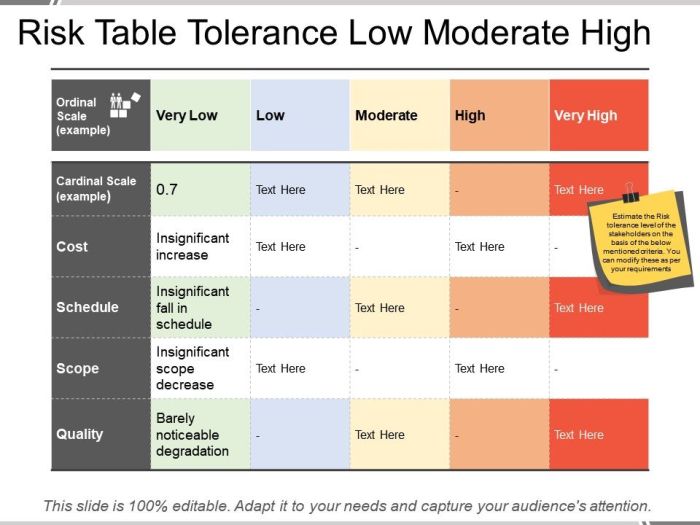
Risk Tolerance in Healthcare

Risk tolerance in the healthcare industry refers to the level of uncertainty or potential risk that an organization is willing to accept in pursuit of its objectives, without compromising patient safety or quality of care.
Factors Influencing Risk Tolerance Level
- Regulatory Environment: Compliance requirements and regulations can shape an organization’s risk tolerance by setting boundaries and standards for patient care.
- Financial Stability: The financial health of an organization can influence its ability to take on risks, as well as its willingness to invest in risk management strategies.
- Organizational Culture: A culture that values innovation and continuous improvement may have a higher risk tolerance compared to a culture that prioritizes stability and tradition.
- Leadership: The tone set by leadership, their risk appetite, and their approach to decision-making can impact the organization’s overall risk tolerance.
Impact on Decision-Making Processes
Risk tolerance can significantly impact decision-making processes in healthcare, influencing how organizations approach issues such as:
- Adopting new technologies and treatments
- Expanding services or entering new markets
- Investing in infrastructure and capital projects
- Responding to crises or emergencies
Risk Mitigation Techniques
In healthcare, risk mitigation techniques are crucial in reducing the likelihood and impact of potential risks. By implementing effective strategies, healthcare organizations can ensure the safety of patients, staff, and the overall quality of care provided.
Prioritizing Risks in Healthcare
Healthcare organizations prioritize risks based on severity and likelihood to determine where to focus their resources and efforts. Risks that pose a higher threat to patient safety or organizational integrity are typically addressed first. By conducting thorough risk assessments, healthcare providers can identify and prioritize risks effectively.
Risk Mitigation Strategies
- Implementing robust quality control measures to prevent errors and ensure compliance with standards and regulations.
- Training staff on proper procedures and protocols to minimize human error and improve patient outcomes.
- Utilizing technology such as electronic health records and telemedicine to enhance communication and streamline processes.
- Developing contingency plans and emergency response protocols to address unexpected events and minimize their impact.
- Engaging in continuous monitoring and evaluation of risks to adapt strategies as needed and stay proactive in risk management.
Challenges in Implementing Risk Mitigation Strategies
- Resistance to change within the organization, making it difficult to implement new processes or technologies.
- Lack of resources or funding to support comprehensive risk mitigation efforts, limiting the organization’s ability to address all potential risks.
- Complex regulatory requirements that can create barriers to effective risk management and compliance.
- Difficulty in predicting and preparing for emerging risks, such as cybersecurity threats or pandemics, which require agility and foresight.
- Balancing risk reduction with the need to maintain efficiency and access to care, as overly stringent risk mitigation measures can impede operations.
In conclusion, navigating risk tolerance in healthcare demands a nuanced approach that considers various factors to make informed decisions and safeguard patient well-being.
Expert Answers
What is risk tolerance in healthcare?
Risk tolerance in healthcare refers to the level of uncertainty that an organization is willing to accept in pursuit of its objectives while ensuring patient safety and quality care.
How do factors influence an organization’s risk tolerance level in healthcare?
Factors such as organizational culture, financial stability, regulatory requirements, and past experiences play a crucial role in shaping an organization’s risk tolerance level in healthcare.
Can risk tolerance impact decision-making processes in healthcare?
Yes, risk tolerance can significantly influence decision-making processes in healthcare by guiding how risks are perceived, assessed, and managed to achieve optimal outcomes for patients and the organization.





